ABSTRACT
Objective: Personal experiences, perceptions, and views of patients are crucial in understanding the subjective impacts of diseases. The complexity and duration of tuberculosis treatment impose significant physical, emotional, social, and economic burdens, highlighting the need for person-centered, integrated care strategies that address stigma, fatigue, and accessibility to support well-being. Patient-reported outcomes (PROs) are essential for capturing patient perspectives and improving health care strategies. In this study we explored the multifaceted experiences of patients with tuberculosis, seeking to understand their values and priorities during treatment. Methods: Semistructured interviews with adult tuberculosis patients were conducted at a referral center for tuberculosis diagnosis and management in northern Portugal. After verbatim transcription and anonymization, thematic analysis was performed. Results: Seventeen interviews were conducted. Most (58.8%) of the study participants were male, and most had pulmonary tuberculosis. Our thematic analysis identified five PROs: treatment experiences; health-related quality of life; functional status; symptoms and symptom burden; and health behaviors. People with tuberculosis acknowledged the impact of multiple factors on their overall health, particularly the psychological and physical burdens of tuberculosis and its treatment. Several areas for improvement and opportunities for enhanced support were identified, particularly in communication, emotional support, and management of treatment burden. Conclusions: Our findings highlight the need for tailored PRO measures (PROMs) addressing treatment burden, psychosocial distress, and functional limitations in tuberculosis care. Enhancing communication, psychological support, and multidisciplinary approaches in tuberculosis management could improve patient outcomes and overall well-being. Addressing tuberculosis-related stigma and providing targeted interventions may contribute to a more people-centered approach to care.
Keywords:
Patient reported outcome measures; Qualitative research; Quality of life; Tuberculosis.
INTRODUCTION Tuberculosis remains a significant global health challenge, affecting approximately 10.8 million individuals worldwide.(1) Despite concerted efforts to mitigate its impact, tuberculosis continues to impose a substantial physical, emotional, and social burden on those affected. (2,3) In Portugal, although tuberculosis incidence has gradually declined over recent decades, it remains a pressing public health concern, with an incidence rate of 13.7 cases per 100,000 population in 2023,(4) underscoring the need for effective and person-centered care strategies.
Although research on the impact of tuberculosis on quality of life is growing, the specific concerns most valued by people with tuberculosis remain underexplored. The prolonged and complex nature of tuberculosis treatment(5) often leads to significant emotional and physical fatigue, disrupting daily life.(3) Although video-observed therapy (VOT) has demonstrated higher patient acceptability than directly observed therapy (DOT),(6) the treatment burden persists, affecting adherence and overall well-being.
The social implications of tuberculosis are equally significant, with stigma and discrimination driven by the contagious nature of the disease frequently leading to social isolation and mental health challenges.(7) The economic burden is also considerable, affecting not only individuals but entire communities.(8) To ensure equitable access to tuberculosis care and support, a person-centered and integrated approach is essential.(1)
Patient-reported outcomes (PROs) are increasingly recognized as valuable in tuberculosis research.(9) Defined as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation by a clinician or anyone else,”(10) PROs provide critical insights into patient experiences. Although PROs are widely studied in chronic diseases such as cancer, diabetes, and HIV,(11) their application in tuberculosis remains limited. A systematic review of cancer-related PROs identified symptom control, physical function, and emotional well-being as key patient concerns.(12) Similarly, tuberculosis research has highlighted the importance of PROs in tailoring treatment and improving patient care.(2) However, existing patient-reported outcome measures (PROMs) are not specifically designed for tuberculosis, limiting their applicability.
Despite progress in qualitative tuberculosis research,(13) most studies on PROs originate from low- or middle-income countries,(14) where findings are often assessed in isolation. Variability in experiences across different phases of treatment remains underexplored, particularly in high-income settings. The present study addressed this gap by examining the experiences of people living with tuberculosis in Portugal, assessing their values and priorities during treatment. By understanding their perspectives, the present study sought to enhance clinical care, develop person-centered strategies, and improve health outcomes for people with tuberculosis.
METHODS This was a qualitative study conducted from May of 2023 to August of 2024 at the Tuberculosis Outpatient Clinic in Vila Nova de Gaia, Portugal. Located in the largest municipality in northern Portugal, the clinic serves as a referral center for confirmed and probable tuberculosis cases in the region. It also manages cases of multidrug-resistant and extensively drug-resistant tuberculosis in the northern and central regions of Portugal. Ethical approval was obtained from the Northern Regional Health Administration in Portugal (Protocol no. CE/2023/77).
People ≥ 18 years of age with a confirmed diagnosis of any type of tuberculosis and currently undergoing treatment were recruited through convenience sampling. Eligible participants were contacted by telephone and invited to participate in an interview, either on a prescheduled date or during their routine follow-up visits. All participants received an information sheet detailing the objectives of the study and how the research team intended to use the results. Before data collection, a male health care professional at the clinic provided a thorough explanation of the study, ensuring that participants had the opportunity to ask questions and clarify any concerns. Written informed consent was obtained from all participants. Those who were unable to provide consent or who declined to participate were excluded.
The semistructured interviews followed a script that was developed by the research team and that was informed by prior studies in the field (see Supplementary material). The script allowed flexibility to explore emerging themes and was pilot tested with five participants, with no subsequent changes thereafter. Participants were asked about various aspects of tuberculosis from their perspective, beginning with their diagnosis, symptoms, and knowledge of the disease. The interviews also explored treatment experiences, including psychosocial implications, challenges related to adherence, and the impact of tuberculosis and its treatment on mental well-being and social interactions. Additionally, participants were asked about their interactions with health care providers, particularly regarding communication patterns and their perceived significance in tuberculosis care.
All interviews were conducted in person at the clinic by the first author (PV), with no other members of the research team present in the room. The first author received training in qualitative research methods from experienced members of the research team (JPR, MV, and PB). Each session lasted approximately 50 minutes.
The interviews were audio-recorded (with participant informed consent) and transcribed verbatim into Portuguese. To ensure confidentiality, all transcripts underwent anonymization, with names, geographic data, and other identifiers being removed in order to prevent data triangulation and patient identification.
A combined inductive and deductive thematic analysis(15) was conducted by two independent researchers (PV and LLF) until meaning saturation was achieved; that is, when no new themes or subthemes (and their underlying relation) emerged.(16) Initially, each transcript was independently reviewed, and a preliminary set of themes and subthemes was developed for each transcript. These were subsequently cross-checked and validated by the research team. The analysis was aimed at identifying commonly reported PROs, including treatment experience, health-related quality of life (HRQoL), functional status, symptoms and symptom burden, and health behaviors, while also allowing room for themes outside this framework. The study was conducted in accordance with the Consolidated Criteria for Reporting Qualitative Research (see Supplementary material).(17)
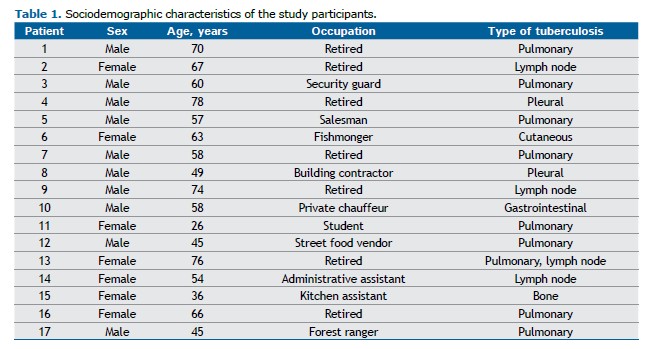
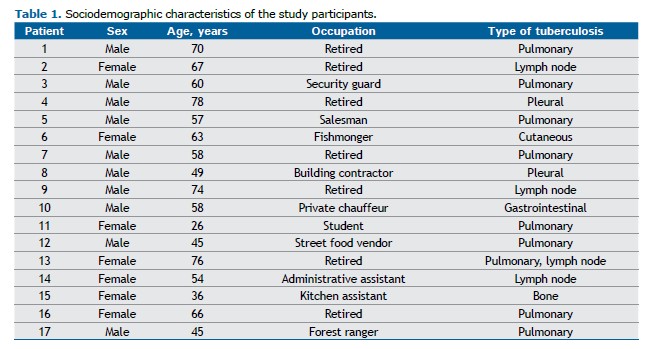
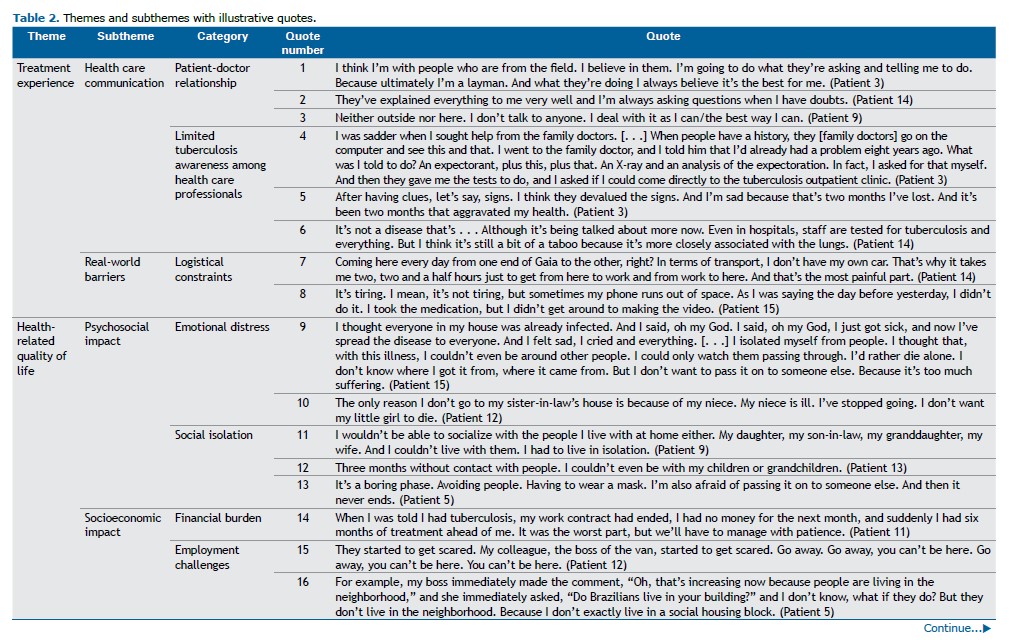
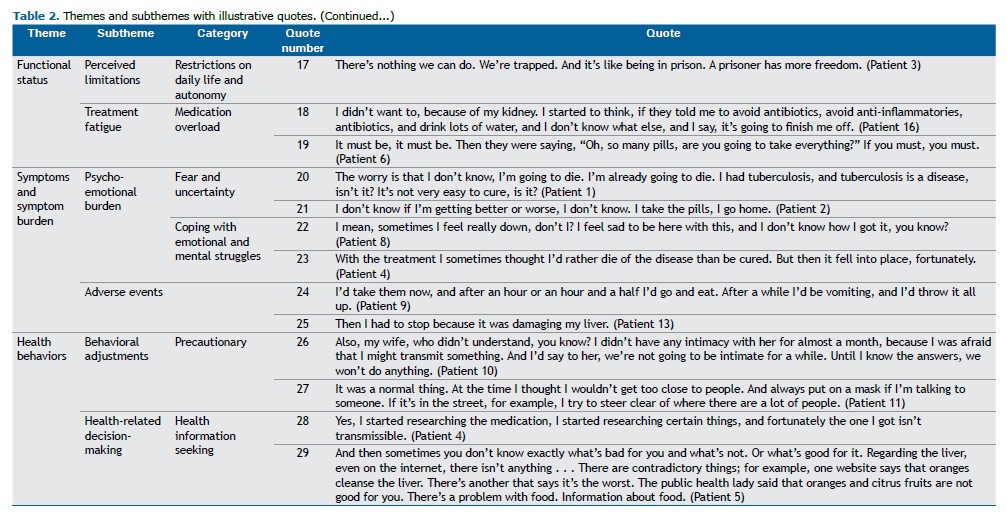
RESULTS A total of 17 participants were interviewed. Of those, 58.8% were male, with a mean age of 57.8 ± 14.2 years. Most of the study participants had pulmonary tuberculosis (n = 8), although other forms of tuberculosis, such as pleural, cutaneous, intestinal, bone, and lymph node tuberculosis, were also present. Eight participants were professionally active, and all resided in the Vila Nova de Gaia municipality. Findings were categorized into five main PROs: treatment experience; HRQoL; functional status; symptoms and symptom burden; and health behaviors. Table 1 shows a detailed description of the sociodemographic characteristics of the study participants.
Participants generally expressed satisfaction with the health care that they received, particularly valuing clear communication from health care professionals (Table 2). Many of the respondents appreciated the support and detailed information provided (see quote number [Q] 1 and Q2; Table 2); however, a subset of patients reported feelings of fear or hesitancy when engaging with health care providers (Q3). The recurring need for more targeted and tuberculosis-specific information was a prominent theme. Diagnostic delays, often attributed to limited awareness among health care professionals, negatively impacted treatment experiences (Q4, Q5, and Q6). Additionally, the burden associated with treatment modalities, particularly in the context of DOT/VOT, was reported to affect adherence and quality of life (Q7 and Q8).
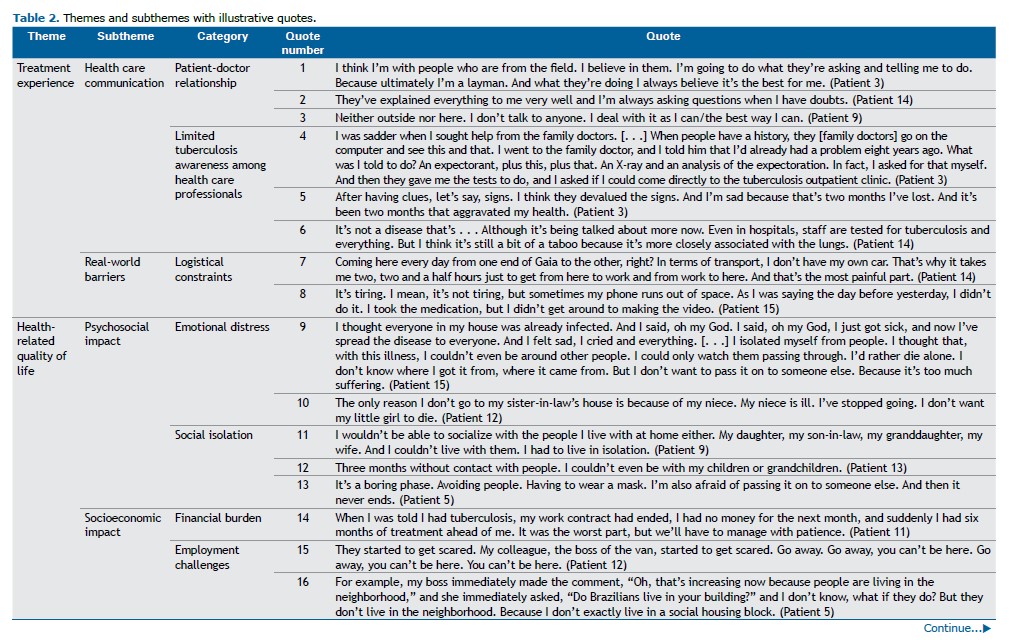
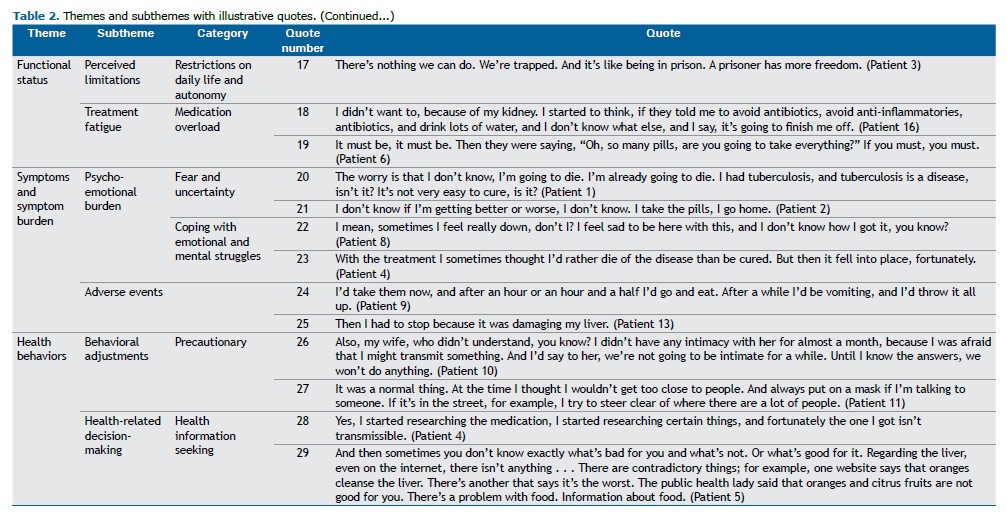
Many of the study participants described significant strain on interpersonal relationships, primarily due to fears surrounding the transmission of tuberculosis. Concerns about infecting loved ones, especially vulnerable individuals such as children and the elderly, led to feelings of isolation, loneliness, and even social exclusion (Q9 and Q10). These experiences reinforced internalized stigma and, in several cases, resulted in self-imposed isolation (Q11 and Q12). Although a few of the study participants managed to resume some of the routines of their daily life, most remained fearful of transmitting the disease, which in turn heightened emotional distress (Q13). The reduction in social interactions was compounded by financial instability, with some participants reporting job loss or diminished economic independence (Q14 and Q15). Furthermore, experiences of discrimination and stigma significantly contributed to psychological distress, thereby reducing HRQoL (Q16).
Tuberculosis symptoms and the treatment process had a tangible impact on participant functional status. Many reported difficulties in performing daily tasks, with a notable perception of lost autonomy (Q17). Concerns regarding the potential impact of tuberculosis on existing comorbid conditions were also voiced (Q18 and Q19). Despite the considerable challenges presented by the disease and its treatment, most of the study participants acknowledged the critical importance of treatment adherence in eventually improving their functional status and alleviating symptoms.
Participants widely acknowledged the severity of tuberculosis and the considerable difficulty associated with its treatment. Uncertainty regarding treatment outcomes, coupled with the fear of medication side effects, further compounded these challenges (Q20 and Q21). The historical association of tuberculosis with high morbidity added to the emotional distress experienced (Q22 and Q23). Many of the study participants expressed concern that adverse side effects could necessitate treatment discontinuation (Q24 and Q25), thereby prolonging the overall recovery process and exacerbating physical and emotional burdens.
Participants changed their health habits because of the disease, exhibiting knowledge regarding transmission routes and the need for personal protective equipment to prevent disease spread (including the use of masks and social distancing as protective measures) and emphasizing adaptation to the new context of social interactions. Although these measures were deemed necessary, they often disrupted the spontaneity of social interactions (Q26), contributing to feelings of isolation (Q27). A proactive approach to seeking tuberculosis-related information was common among participants (Q28 and Q29), and many believed that greater knowledge could help alleviate some of the distress associated with the disease. Notably, although participants expressed a desire for guidance on managing lifestyle changes, particularly regarding nutrition, there was a prevailing sentiment that support from health care professionals in this area was insufficient.
DISCUSSION Our qualitative analysis revealed key insights into psychosocial and health care experiences of people undergoing tuberculosis treatment, highlighting their understanding of tuberculosis and its social and economic impacts, as well as the psychological burden of tuberculosis treatment.
A major PRO identified in the present study centered on treatment experiences, highlighting essential factors for people with tuberculosis, with the need for clear communication playing a crucial role. Although many of the study participants valued the information and support provided by health care professionals—which reassured them throughout the treatment process(18)—others expressed hesitancy or fear in communicating openly, leading to gaps in understanding and emotional distress. This underscores the need for person-centered communication strategies that address medical and psychological needs. Tuberculosis awareness also significantly influenced the overall treatment experience. The literature reiterates that although tuberculosis knowledge is adequate in several health care professional groups, continued efforts are needed to keep this knowledge updated.(19) Our findings suggest that a lack of awareness among health care professionals contributes to diagnostic delay,(20) emphasizing the importance of continued training and education for improved PROs.
Tuberculosis had a profound impact on HRQoL, a dimension known to be deeply affected in people with tuberculosis.(21) Many of the study participants reported anxiety, fear, and emotional distress, which persisted even after starting adequate treatment. The most significant impact stemmed from limitations in social relationships, particularly with close family members. Many of the study participants isolated themselves from loved ones to prevent transmission, particularly to vulnerable individuals such as children and the elderly, with the sense of isolation—both physical (as a result of mandatory isolation) and social (from stigma and reduced social contact)—worsening emotional distress.
Tuberculosis treatment also imposed a loss of freedom, restricting their ability to work, travel, or engage in daily activities, further affecting HRQoL. Combined with the physical and psychological burden, these factors had a profound impact on the overall well-being of the study participants, highlighting the need for targeted interventions to enhance patient care.(22)
Financial instability was a major concern, given that prolonged treatment led to loss of employment or income. This financial stress added another layer of difficulty to an already challenging situation, with improved social support and the involvement of family and community members in tuberculosis treatment emerging as critical in addressing this issue.(18)
Stigma and discrimination emerged as another significant factor influencing social interactions and HRQoL, with participants experiencing discrimination from peers, coworkers, and even family members due to misconceptions about tuberculosis transmission. These findings are consistent with those of previous studies highlighting the persistent stigma associated with tuberculosis and its detrimental effects on social well-being.(7)
Functional status was widely recognized as an important outcome, with tuberculosis and its treatment significantly affecting physical abilities. Although the functional impact of tuberculosis sequelae is well documented,(23) the impact of active tuberculosis on daily living remains underrepresented in the literature. Participants highlighted the burden of symptoms on daily activities, contributing to psychological and physical distress. Despite these challenges, most remained adherent to treatment, recognizing its necessity. Providing adequate support and education on the impact of tuberculosis on daily function could enhance PROs.
The perception of tuberculosis as a difficult-to-treat disease with a demanding treatment regimen emerged as a key determinant of outcomes, with participants expressing frustration over its complexity and duration. Concerns over medication side effects and uncertainty regarding treatment effectiveness contributed to emotional fatigue, further exacerbating mental health challenges. Although DOT and VOT remain essential for tuberculosis management,(24,25) they impose social, financial, and occupational burdens, for which more patient-friendly approaches should be explored.(26)
Although participants recognized the importance of adherence, fear of potential side effects had a profound impact on their well-being. A structured support network focusing on early identification and management of side effects could ease concerns. Multidisciplinary care, involving physicians, nurses, and social workers,(27) and, as suggested by our data, the need for nutritional support were highlighted as essential for comprehensive tuberculosis management.
Changes in health behaviors were also noted, with participants demonstrating increased awareness and understanding of tuberculosis transmission and preventive measures, including mask wearing and social distancing. Although these behaviors are necessary for infection control, they exacerbated feelings of isolation and psychological distress. Knowledge gaps regarding tuberculosis persisted,(28) with some of the study participants attempting to self-educate, emphasizing the need for structured education and accessible information to improve support and understanding during tuberculosis treatment.
Our study provides valuable insights into the experiences of people with tuberculosis, capturing multiple dimensions of their health outcomes. Given that most of the studies on similar topics have been conducted in low- or middle-income countries, our findings contribute perspectives from different health care settings, allowing broader comparisons. The wide range of themes explored enabled a comprehensive assessment of participant experiences and needs. However, some limitations must be acknowledged. We were unable to conduct member checking to validate participant responses; this could have strengthened the reliability of our findings. Additionally, because we used convenience sampling, selection bias may have excluded individuals with lower engagement in their treatment, limiting the diversity of perspectives. Recall bias and the self-reported nature of the data may also have influenced responses, as participants may have omitted or emphasized certain experiences.
The findings of the present study have several important implications for health care providers and policymakers. Each of the identified domains had a significant impact on the overall well-being of patients and could serve as key areas for a more personalized treatment approach targeting enhanced patient outcomes and satisfaction. Improving tuberculosis-related information is crucial not only for people with tuberculosis, given that increased knowledge may ease disease burden, but also for health care professionals, given that enhanced training could increase awareness and lead to improved care. Strengthening patient-provider communication and multidisciplinary support—including nutritional support and psychological support to help patients cope with the emotional distress—could further enhance integrated care. Social determinants must also be considered. Financial assistance and employment protection could help alleviate economic strain, while public health campaigns aimed at reducing tuberculosis-related stigma could foster a more supportive environment. Further research on PROs in tuberculosis care, particularly in high-income settings, is needed. Developing tuberculosis-specific PROMs can promote a person-centered approach, ensuring that treatment aligns with the lived experiences and priorities of people with tuberculosis.
AUTHOR CONTRIBUTIONS PV: conceptualization, data curation, formal analysis, investigation, methodology, visualization, writing—original draft, and writing—review and editing; LL: formal analysis, visualization, writing—original draft, and writing—review and editing; MV and JPR: conceptualization, formal analysis, methodology, resources, supervision, validation, visualization, and writing—review and editing; PB: conceptualization, methodology, visualization, and writing—review and editing; and RD: conceptualization, project administration, supervision, validation, and writing—review and editing. All authors read and approved the final manuscript.
CONFLICTS OF INTEREST None declared.
REFERENCES 1. World Health Organization (WHO) [homepage on the Internet]. Geneva: WHO; c2024 [updated 2024 Oct 29; cited 2025 May 1]. Global Tuberculosis Report 2024. https://www.who.int/publications/i/item/9789240101531
2. Margineanu I, Butnaru T, Lam M, Baiceanu D, Dragomir R, Arbore AS, et al. Tuberculosis impacts multiple aspects in quality of life in a Romanian cohort of drug-susceptible and drug resistant patients: A patient-reported outcome measures study. Trop Med Int Health. 2024;29(7):584-593. https://doi.org/10.1111/tmi.13996
3. Guo N, Marra CA, Marra F, Moadebi S, Elwood RK, Fitzgerald JM. Health state utilities in latent and active tuberculosis. Value Health. 2008;11(7):1154-61. https://doi.org/10.1111/j.1524-4733.2008.00355.x
4. Portugal. Ministério da Saúde. Direção-Geral da Saúde (DGS) [homepage on the Internet]. Lisboa: DGS; c2025 [cited 2025 May 1]. Relatório de Vigilância e Monitorização da Tuberculose em Portugal: Dados 2023. Available from: https://www.dgs.pt/em-destaque/tuberculose-em-portugal-mantem-se-estavel-pdf.aspx
5. World Health Organization (WHO) [homepage on the Internet]. Geneva: WHO; c2023 [updated 2020 Jun 15; cited 2025 May 1] WHO consolidated guidelines on tuberculosis: Module 4: Treatment: Drug-resistant tuberculosis treatment. Available from: https://www.who.int/publications/i/item/9789240048126
6. Chen EC, Owaisi R, Goldschmidt L, Maimets IK, Daftary A. Patient perceptions of video directly observed therapy for tuberculosis: a systematic review. J Clin Tuberc Other Mycobact Dis. 2023;35:100406. https://doi.org/10.1016/j.jctube.2023.100406
7. DeSanto D, Velen K, Lessells R, Makgopa S, Gumede D, Fielding K, et al. A qualitative exploration into the presence of TB stigmatization across three districts in South Africa. BMC Public Health. 2023;23(1):504. https://doi.org/10.1186/s12889-023-15407-2
8. Ananthakrishnan R, Jeyaraj A, Palani G, Sathiyasekaran BW. Socioeconomic impact of TB on patients registered within RNTCP and their families in the year 2007 in Chennai, India. Lung India. 2012;29(3):221-6. https://doi.org/10.4103/0970-2113.99103
9. Martín D, Barbosa P, Ramos JP, Vieira M, Duarte R. People first: a participatory community approach on patient-reported outcomes in tuberculosis. Breathe (Sheff). 2024;20(1):230138. https://doi.org/10.1183/20734735.0138-2023
10. U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79. https://doi.org/10.1186/1477-7525-4-79
11. Kall M, Marcellin F, Harding R, Lazarus JV, Carrieri P. Patient-reported outcomes to enhance person-centred HIV care. Lancet HIV. 2020;7(1):e59-e68. https://doi.org/10.1016/S2352-3018(19)30345-5
12. Basch E, Schrag D, Henson S, Jansen J, Ginos B, Stover AM, et al. Effect of Electronic Symptom Monitoring on Patient-Reported Outcomes Among Patients With Metastatic Cancer: A Randomized Clinical Trial. JAMA. 2022;327(24):2413-2422. https://doi.org/10.1001/jama.2022.9265
13. Addo J, Pearce D, Metcalf M, Lundquist C, Thomas G, Barros-Aguirre D, et al. Living with tuberculosis: a qualitative study of patients’ experiences with disease and treatment. BMC Public Health. 2022;22(1):1717. https://doi.org/10.1186/s12889-022-14115-7
14. Cazabon D, Pande T, Sen P, Daftary A, Arsenault C, Bhatnagar H, et al. User experience and patient satisfaction with tuberculosis care in low- and middle-income countries: A systematic review. J Clin Tuberc Other Mycobact Dis. 2020;19:100154. https://doi.org/10.1016/j.jctube.2020.100154
15. Braun V, Clarke V. Thematic analysis: a practical guide. California: SAGE Publishing; 2022. https://doi.org/10.53841/bpsqmip.2022.1.33.46
16. Hennink MM, Kaiser BN, Marconi VC. Code Saturation Versus Meaning Saturation: How Many Interviews Are Enough? Qual Health Res. 2017;27(4):591-608. https://doi.org/10.1177/1049732316665344
17. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-57. https://doi.org/10.1093/intqhc/mzm042
18. Dilas D, Flores R, Morales-García WC, Calizaya-Milla YE, Morales-García M, Sairitupa-Sanchez L, et al. Social Support, Quality of Care, and Patient Adherence to Tuberculosis Treatment in Peru: The Mediating Role of Nurse Health Education. Patient Prefer Adherence. 2023;17:175-186. https://doi.org/10.2147/PPA.S391930
19. Wondimu W, Yosef T, Gebremedhin T, Hailemariam N. Health professionals’ knowledge and attitude of tuberculosis infection control in Mizan Tepi University Teaching Hospital, Ethiopia. J Clin Tuberc Other Mycobact Dis. 2021;24:100239. https://doi.org/10.1016/j.jctube.2021.100239
20. Silva T, Aguiar A, Gomes A, Marques M, Pereira C, Rodrigues R, et al. Delays have dangerous ends: Tuberculosis diagnosis delay in Portugal, a qualitative study. Pulmonology. 2024;30(6):653-658. https://doi.org/10.1016/j.pulmoe.2024.02.006
21. Yasobant S, Khatib MN, Syed ZQ, Gaidhane AM, Shah H, Narkhede K, et al. Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review. Infect Dis Rep. 2022;14(4):509-524. https://doi.org/10.3390/idr14040055
22. Bauer M, Ahmed S, Benedetti A, Greenaway C, Lalli M, Leavens A, et al. Health-related quality of life and tuberculosis: a longitudinal cohort study. Health Qual Life Outcomes. 2015;13:65. https://doi.org/10.1186/s12955-015-0250-4
23. Di Naso FC, Pereira JS, Schuh SJ, Unis G. Functional evaluation in patients with pulmonary tuberculosis sequelae [Article in Portuguese]. Rev Port Pneumol. 2011;17(5):216-21. https://doi.org/10.1016/j.rppneu.2011.06.010
24. Saukkonen JJ, Duarte R, Munsiff SS, Winston CA, Mammen MJ, Abubakar I, et al. Updates on the Treatment of Drug-Susceptible and Drug-Resistant Tuberculosis: An Official ATS/CDC/ERS/IDSA Clinical Practice Guideline. Am J Respir Crit Care Med. 2024;211(1):15-33. https://doi.org/10.1164/rccm.202410-2096ST
25. Mangan JM, Woodruff RS, Winston CA, Nabity SA, Haddad MB, et al. Recommendations for Use of Video Directly Observed Therapy During Tuberculosis Treatment - United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72(12):313-316. https://doi.org/10.15585/mmwr.mm7212a4
26. Kumari U, Wasim U, Kumari S, Khoshbakht F. Electronic directly observed therapy (eDOT) therapy: a digital breakthrough in tuberculosis treatment - A commentary. Ann Med Surg (Lond). 2023;85(5):2268-2269. https://doi.org/10.1097/MS9.0000000000000668
27. Ramos JP, Vieira M, Pimentel C, Argel M, Barbosa P, Duarte R. Building bridges: multidisciplinary teams in tuberculosis prevention and care. Breathe (Sheff). 2023;19(3):230092. https://doi.org/10.1183/20734735.0092-2023
28. Lobie TA, Roba AA. Tuberculosis knowledge gaps and associated factors among suspects of tuberculosis in a peripheral emerging region of northwest Ethiopia: a case of Benishangul Gumuz. medRxiv. 2022. https://doi.org/10.1101/2022.07.11.22277486


 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Pocket
Pocket